For the last few years my sleep has been less effective and less restful. I feel more tired and fatigued in the day and I yawn more frequently. Another symptom that has started in the last year is higher blood pressure and recently being diagnosed with hypertension. I was getting tired of being tired. This is my journey of figuring out what I had and what things could I do to help get a better night’s sleep and fix the underlying cause.
One of the most common problems of poor sleep is Obstructive Sleep Apnea. OSA affected 6.37 million Americans in 2016 and this study has shown an increase in family practice diagnosis over the years. It is thought that many people have yet to be diagnosed. When you look at the associated risks of having OSA it is actually quite scary. For myself having a blood pressure of 165/115 without having my arm cut off and simply sitting at a table is not cool! Hypertension is linked with OSA and this was one of the clues that made me start putting the pieces together.
Associated Symptoms of Obstructive Sleep Apnea
Chronic Snoring
Gasping Episodes
Daytime Drowsiness
Headaches
Chronic Pain
Obesity or over weight
Hypertension
Anxiety, Mood Swings, Fatigue and/or Depression
Chronic Allergies
Academic Challenges
Hyper-activity
Asthma
Attention Deficit
Hypothyroidism
Crooked Teeth or Crowded Teeth
Taken from Hollowbrook Sleep.
Now these symptoms can have a different cause and there are others like GERD that are associated with OSA. Another thing to note is that with hypertension comes its own cmplications. Shortened life span, stroke, cardiac/heart issues, and more. I am definitely invested in figuring this out!
Years ago I had the opportunity to hear a speaker on Obstructive Sleep Apnea. His name was David Singh DMD PhD. He was sharing his research on treating OSA by improving the airway by changing one thing, the upper arch or maxilla. Through 3D volume rendering of the airway, skull and jaw with cone beam CT and epigenetics OSA in kids and adults were being fixed. After the conference I was able to spend some time with Dr. Singh. He looked at my face and told me that I was at risk for OSA. This was the first puzzle piece in my diagnosis of OSA, a narrow maxillary arch, poor development of the mid face or maxillary bone, and tooth crowding.

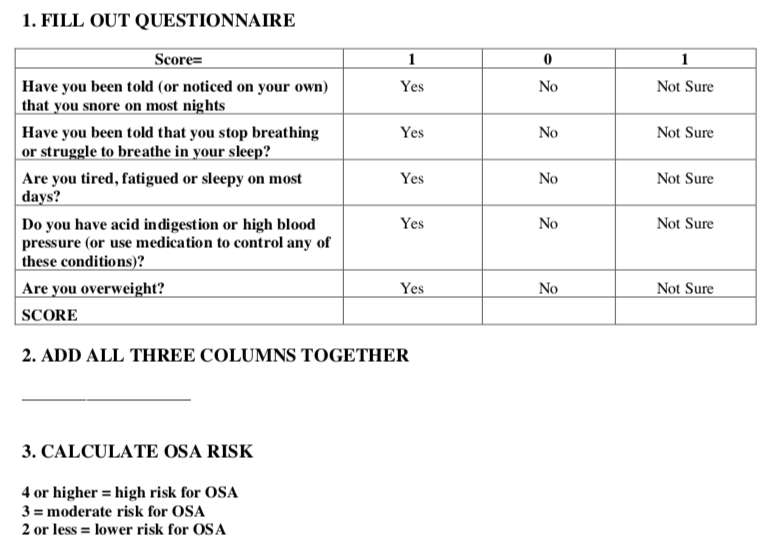
The GASP Questionnaire is a tool that I have used to guide further screening. It consists of 5 questions. Over the years this questionnaire has scored higher and now I am at 5/5. I find this a useful start in talking about OSA.
Check Your Uvula
Another thing to look for, and this is more for the medical practitioner but it is something anyone can try, is to see how far down your soft palate or uvula covers the back of your throat. Ever wonder why your doctor was looking into your mouth? One of the reasons was to see the shape of your soft palate. Now the primary reason for looking is for redness and possible infection, but the quality of your airway is also important. This is called the Mallampati Score Mallampati Score and mostly used by anesthesiologists.
Check for Clenching
While you are looking in your mouth there are two signs that are important to pick up. The first is a callous formation in the inside of your cheeks running horizontal on one or both sides. This ridge is something we can feel with our tongue and means that we are excessively clenching. We call this linea alba. Now you might say, “I don’t clench.” But if you have this sign or callous that means that this is happening. Most likely it is while you are asleep.
Feel the inside of your cheeks. Do you feel a line or ridge? Look for any bumps as well.
If you have this then you are clenching, a lot!
The next is tooth marks on the tongue. These are called ruggae and they can mean a couple of things. One is that it is another sign of clenching and is usually associated with linea alba. It can also mean poor tongue control and a tongue thrust. It can also mean that your upper arch is too small or narrow.
Check and check. I have both.
I think I may have OSA. What should I do?
There are a few things you can do to start. Dr. Robert Vogt is a family medicine physician in Colorado Springs who starts his sleep screening with an overnight pulse oxygen reading. Here is the company that they use. VPOD Ultra
Based on this test they determine if a sleep study is necessary.
I decided to go straight to a sleep study. For 125 dollars I conducted an in home sleep study measuring breathing, oxygenation of my blood, heart rate, movement and snoring. I wore my Apple Watch on the other wrist to do a comparison. I've always been curious to see if a smart watch can accurately track my sleep.
To be Continued…