Sometimes it is appropriate to order imaging for a TMJ problem or TMD.
Reasons to order imaging
There is joint crepitus or grinding with pain. (Panorex, Tomograph, or Cone Beam CT)
You have a locked TMJ that is not improving with treatment. (Cone Beam CT or MRI)
Screening for other conditions that can cause pain such as a sinus infection. (Cone Beam CT or MRI)
Sleep Questionnaire is positive and you are checking the airway. (Cone Beam CT)
Other reasons that are common are related to the approach used by the dentist for their TMJ evaluation. TMJ orientation as well as skull, jaw and neck morphology have been used to guide treatment and can be unique to the various philosophies of TMD evaluation and treatment.
Radiology
What tests are available?
Panorex
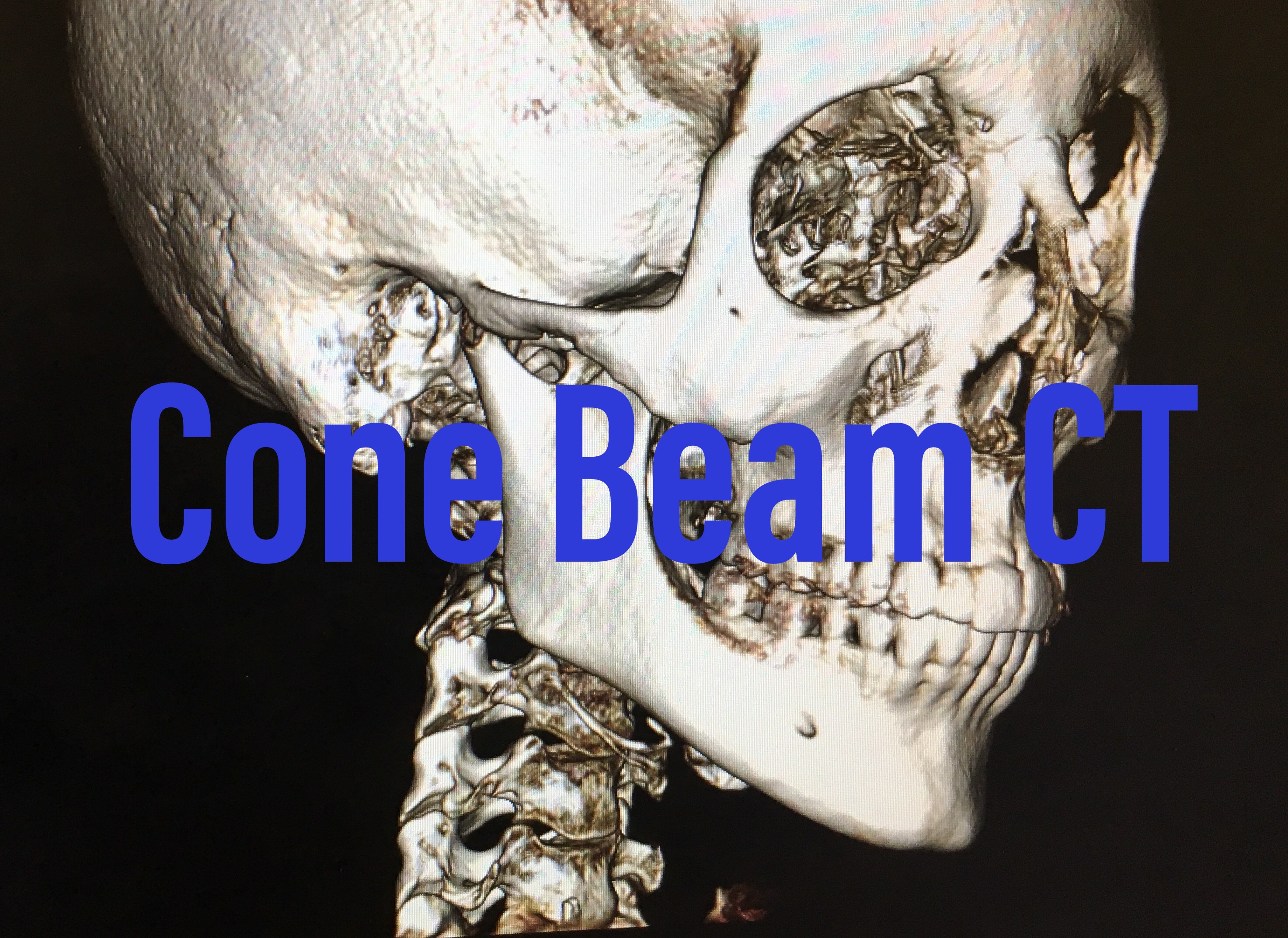
Cone Beam CT
MRI
Diagnostic Ultrasound

Panorex
A Panorex is a great screening tool but there is distortion as well as potential bony overlay that will limit the view of the TMJ’s. The arc and path of the machine increases the 'size' of the condyle and reverses the condylar poles. (What you think is the lateral pole is actually the medial or inside pole of the condylar head) It is used as a screening tool to see if there are condylar fractures or condylar head degenerative changes.
Pros and Cons
Quick imaging and accessible.
Distorts the condyles of the mandible.
There is bony overlay making it harder to see the condylar head.
2D
Similar studies
Tomograph is a cyclical TMJ imaging device that creates a clearer picture but is still two dimensional.
Lateral cephalometric for skull, jaw, tooth and cervical positioning. Primarily used in orthodontics and is focused on neutral angles of the head, jaw, teeth, hyoid and neck.
Cone Beam CT
This has become the standard of practice for TMJ imaging. There is no distortion and we have a 3D image of the skull, jaw and neck, including the airway. The teeth, mandible, TMJ, airway, sinuses, skull, and cervical spine are imaged in sections as well as in three dimensions. Soft tissue visualization is limited and disc placement is inferred. For soft tissue integrity and disc injuries an open and closed TMJ MRI is recommended.
Pros and Cons
There is radiation but this is much lower than a medical CT
Limited soft tissue view
Can be done quickly. Takes minutes.
Lots of data!
3D

TMJ MRI
This is great to determine swelling in the joint as well as disc placement and even an adhered TMJ disc to the eminence. A corrected view is ordered to line up with the orientation of the TMJ. These joints are angled inward but can have different orientations so a scouting film is needed. Looking at an open mouth and closed view is necessary as well as para-coronal and para-sagittal views with minimal spacing between each slice.
An MRI is more limited to assess bony changes but has no radiation.
More expensive and takes more time to do.
Are we going to use the information that an MRI gives us?
If we already know we have a swollen and inflamed joint does seeing this on an MRI change our treatment?
Reasons to do a TMJ MRI
Suspect an adhered disc to the eminence and are considering a maxillofacial surgical consult.
Disc shape and placement is compromised and preventing progression of treatment.
Our treatment will change based on what we find.

Diagnostic Ultrasound
Diagnostic Ultrasound for TMJ issues is fairly recent with only a handful of studies being done so far. We can get a sense of TMJ motion, condylar neck and head integrity, swelling in the joint, and even disc position. This takes a lot of skill from the practitioner but it is very quick and can be done in the practitioner’s clinic. There is no radiation and it is safe to use. This is a an imaging tool that will continue to grow in prominence as accessibility is increasing.
Whatever imaging you decide to order it is important for the clinician to view the actual images and not rely on a report. Radiology reporting on TMJ imaging is not always done be a maxillofacial trained radiologist and data can be missed.